To a very great extent, simulation is the future of surgery. Within a few years, no surgical procedure will be performed without first perfecting it on a full-sized, 3D, and possibly haptic simulation of the specific patient; and most surgical training and skills assessment will be conducted on simulators.
Recognizing that this is the future of surgery, the Department is actively involved in the research and development of simulation technologies both within the Department and in partnership with both global and local hardware engineering and software development corporations.
Ultrasound Simulator
The surgery faculty, through SEMCE, teach both a basic and advanced US simulation course. To learn ultrasound skills medical students usually use real portable ultrasound machines on crude, short-lived, gel-and-noodles models of the abdomen. The machines are expensive, and the models are time consuming for the surgeon-teacher to build and therefore expensive also. Measuring/monitoring the students as they practice requires direct expert observation and manual recording of performance and is therefore expensive. Teaching by demonstration requires one-on-one learner to educator.
The Department has developed an ultrasound simulator with a dummy probe whose position is tracked with 6 degrees of freedom as it is manipulated in contact with a physical model of the abdomen. The coordinate data stream will be used to interrogate a virtual digitized model of the abdomen, resulting in an image that varies in real time with the probe position.
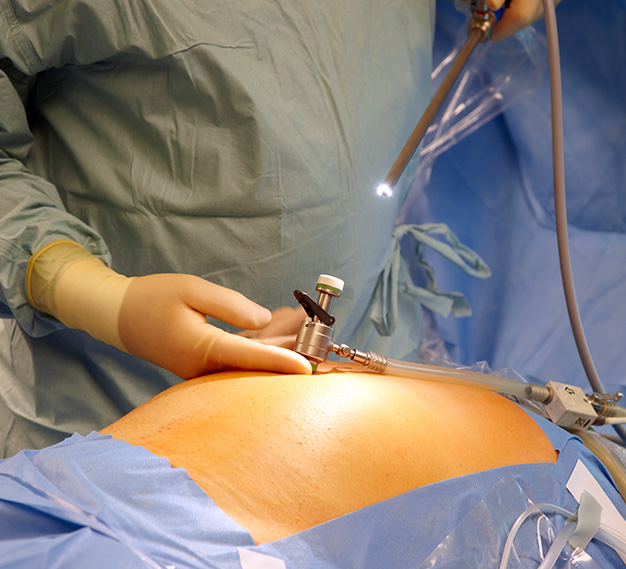
Fundamentals of Laparoscopic Surgery (FLS)
Official Testing Center The Department of Surgery at Wayne State University/Detroit Medical Center is an official testing center for surgeons and general surgery residents who are interested in becoming certified in the Fundamentals of Laparoscopic Surgery (FLS). More than 100 residents and surgeons have undergone FLS certification testing since 2007. Currently the Department of Surgery has 2 FLS certified test proctors.
Fundamentals of Endoscopic Surgery (FES)
Official Testing Center The Department of Surgery at Wayne State University/Detroit Medical Center is one of two sites in Michigan designated as an official testing center for surgeons and general surgery residents who are interested in becoming certified in the Fundamentals of Endoscopic Surgery (FES). Currently we are doing over 20 tests a year with two proctors.
Contact:
David A. Edelman, M.D., Director, Clinical Professor of Surgery, Educational Planner
Phone: 313-745-7514
E-mail: dedelman@med.wayne.edu
Simulation, Scoring, and Proficiency Monitoring System
The Department of Surgery has 4 FLS machines associated with a Simulation Support Platform that allows us to record and score all practice attempts of FLS. We have over 10,000 trials saved.
Surgical Skills and Simulation Center The Department of Surgery has a surgical skills and simulation training laboratory (established in 2007) to further enhance the teaching of open, laparoscopic, endoscopic and endovascular surgical skills of medical students, residents, fellows, allied health professionals, academic faculty and community physicians alike. The Department has designed their own curriculum that is used by both the MS4s (ACES) and the PGY-1 residents.
Contact:
David A. Edelman, M.D., Director, Clinical Professor of Surgery, Educational Planner
Phone: 313-745-7514
E-mail: dedelman@med.wayne.edu
Patient Specific Surgical Simulation
The Department is developing a patient-specific surgical simulator. The simulations, based on 64-slice CT images, will enable surgeons to plan and practice virtual procedures on models of their actual individual patients. The project has reached proof-of-concept stage..